Are You Being Conned By Caltrate?
If you go to your Doctor and they happen to prescribe you with a Calcium supplement, it is likely that they will recommend the popular pharmacy brand ‘Caltrate’. So, does this Calcium supplement stack up?

Is Caltrate worth the money that droves of Australians spend to increase their calcium levels, protect their bones, and prevent disease?
The research points to no.
Different forms of calcium vary in their bioavailability. Calcium carbonate (the form found in Caltrate) is poorly absorbed by the body.
So why do we persist in stocking it, prescribing it and taking it if our bodies struggle to process and utilise it?
The Caltrate website compares calcium carbonate with another form of calcium, calcium citrate.
The people at Caltrate declare that they use “a concentrated form of calcium, yielding about twice the amount of elemental calcium than equal amounts of calcium citrate” and therefore “you can take fewer tablets to get the recommended amounts of calcium…and fewer tablets mean your bottle of Caltrate may last longer”.
So they’re all about our bottom line?
Unfortunately they don’t mention that calcium carbonate tablets need a significant amount of stomach acid to be absorbed and therefore must be taken with meals (or about a litre of orange juice!), whereas calcium citrate tablets don’t have this limitation.
Not only that, but a recent study has shown calcium citrate raises plasma calcium concentrations by 94% more than calcium carbonate in postmenopausal women.
The same study determined that calcium citrate decreased markers of bone resorption (where your body leaches calcium from your bones) significantly more than calcium carbonate.
These findings support an older meta-analysis that proved calcium citrate is better absorbed than calcium carbonate by approximately 22-27%. The results were irrespective of whether supplements were taken on an empty stomach or with meals.
Another recent study was conducted at Purdue University and showed that dairy products were better for bones than calcium carbonate supplements.
Connie Weaver, professor and head of the Food and Nutrition Department, found that the bones of rats fed nonfat dry milk were longer, wider, more dense and stronger than those of rats fed a diet with calcium carbonate.
Weaver said that this result was “not due to increased calcium absorption. It’s more about protecting against bones losing calcium, according to our results of calcium metabolism. Bones are in constant turnover, especially when they are growing. Youth need to have bone formation outweigh bone loss.”
This is where calcium carbonate really falls down.
Calcium citrate has already demonstrated a greater ability to decreased bone resorption than calcium carbonate. However, the type of calcium that really excels in this department is calcium hydroxyapatite.
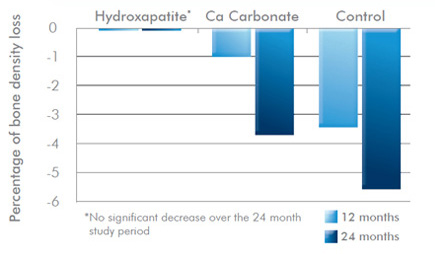
The Hydroxyapatite form of Calcium appears to Reduce Bone Mineral Density Loss Better than Any Other Form
In a two year study involving 60 postmenopausal women, only the group given hydroxyapatite maintained bone mineral density, while the calcium carbonate group and placebo group encountered a significant and alarming reduction in bone mineral density.
See the below graph for the results.
So why is it that hydroxyapatite calcium is so much better than the rest? Basically because it is easy to absorb and is the same type of calcium mainly found in our bones.
Or, for a more complicated explanation for you young Einsteins out there, please see the next two paragraphs…
The mineral phase of bone extracellular matrix is a combination of lots of amorphous and crystalline states, mainly hydroxyapatite crystals. Out of the total amount of calcium in the body, 99% is found together with phosphorus in bones and teeth as hydroxyapatite. The hydroxyapatite form of calcium makes up about 70% of the weight of bone.
Osteoblasts (originate in the bone marrow and contribute to the production of new bone), under the control of parathyroid hormone, vitamin D and oestrogen, secrete proteins which attract calcium circulating in the blood. Calcium, phosphorus and magnesium bind to the surface of the bone, forming hydroxyapatite crystals. These crystals form and strengthen new bone.
The Spinal Centre Comment:
Fundamentally, when you look at all the evidence, Caltrate is not worth taking when there are much better supplements out there.
It uses a form of calcium that doesn’t get absorbed easily and isn’t anywhere near as good for bone health as other forms of calcium, particularly hydroxyapatite.
Calcium is an important mineral, and not just for bone health. If you have an increased need for calcium and wish to supplement then don’t waste your money on a low quality product.
The body requires calcium for the proper functioning of many processes including muscle contraction, nerve conduction, beating of the heart, hormone release, blood coagulation, energy production and maintenance of immune function. It is essential for bone and teeth mineralisation.
Low calcium states are associated with some serious diseases such as colorectal cancer, osteoporosis, hypertension, pre-eclampsia and eclampsia.
In June 2010 a large Italian study showed that postmenopausal women who had a low calcium intake had a significantly higher risk of developing both osteoporosis and hypertension.
“Our study confirms that there may be a link between hypertension and low bone mass and that a low calcium intake could be a risk factor for the development of osteoporosis in postmenopausal women” said Professor Maria Manara, Department of Rheumatology, Gaetano Pini Institute, Milan, Italy, and lead author of the study.
This and other research has shown calcium has a role in prevention of diseases such as osteoporosis. Also, calcium supplementation is traditionally used to avoid or correct deficiency states. Interestingly, calcium can also be used successfully to manage other conditions, like PMS.
Speak to Dr. Hooper or our Naturopath Nadia (in Hawthorn) about your calcium requirements at your next appointment.
Calcium is essential for health and wellbeing. It is considered a critical nutrient in children, pregnant women and postmenopausal women.
Education in terms of which supplement to take and why seems to be generally lacking and substandard Caltrate seems to be everywhere.
Now you know better, so take a better form of calcium. It is important to opt for quality not quantity and see the benefits good supplementation can have for your health.
Bioceuticals AdvaCal Forte, Metagenics Calcitite Hi-Strength and Metagenics OsteoPlus are great calcium supplements we stock at The Spinal Centre.
And guess what? They actually work.
Remember that calcium can interact with numerous drugs and should be used with caution by people with renal disease or hyperparathyroid conditions.
What else can I do?
Ensure you have an adequate intake of dietary calcium. Don’t just think dairy!
You can find calcium in almonds, broccoli, buckwheat, dairy, egg yolk, figs, kale, fish paste, green leafy vegetables, molasses, prawns, salmon, sardines, anchovies, seaweed, sesame seeds, snapper, soybeans, tahini, tofu, turnips and more…

Know how much calcium you need – You may need more calcium if you fall into any of the following categories:
- Ageing
- Excessive alcohol intake
- Increased bed rest
- Bone fractures
- High caffeine intake
- Chronic vitamin C deficiency
- Diuretic use
- Depression
- Excessive fat intake
- High blood pressure
- High phosphate intake
- High protein and sugar diets
- High sodium intake
- Hypoglycaemia
- Hypothyroidism
- Lack of exercise
- Lactation or pregnancy
- Magnesium deficiency
- Post menopause
Final thoughts
Know your supplements
Choose a supplement with a hydroxyapatite and / or citrate form of calcium.
Make sure you check the amount of elemental calcium in a supplement; that’s what your body will actually use.
Don’t take a whole lot of calcium at once, it is better to take several smaller doses per day.
Your body needs co-factors such as vitamin D to use calcium most efficiently, so look for calcium supplements that contain both.
References
Albertazzi P, Steel SA, Howarth EM & Purdie DW 2004, ‘Comparison of the effects of two different types of calcium supplementation on markers of bone metabolism in a postmenopausal osteopenic population with low calcium intake: a double-blind placebo-controlled trial’, Climacteric, vol. 7, no. 1, pp. 33-40.
Castelo-Branco C, Pons F, Vicente JJ, Sanjuan A & Vanrell JA 1999, ‘Preventing postmenopausal bone loss with ossein-hydroxyapatite compounds. Results of a two-year, prospective trial’, J Reprod Med, vol. 44, no. 7, pp. 601-605.
European League Against Rheumatism 2010, ‘Low calcium intake linked with increased risk of osteoporosis and hypertension in postmenopausal women’, ScienceDaily, Retrieved October 25, 2010, from http://www.sciencedaily.com/releases/2010/06/100617102412
Fernández-Pareja A, Hernández-Blanco E, Pérez-Maceda JM, Riera Rubio VJ, Palazuelos JH & Dalmau JM 2007, ‘Prevention of osteoporosis: four-year follow-up of a cohort of postmenopausal women treated with an ossein-hydroxyapatite compound’, Clin Drug Investig, vol. 27, no. 4, pp. 227-232.
Ruegsegger P, Keller A & Dambacher MA 1995, ‘Comparison of the treatment effects of ossein-hydroxyapatite compound and calcium carbonate in osteoporotic females’, Osteoporosis Int, vol. 5, pp. 30-34.
Shea B et al 2002, ‘Osteoporosis Methodology Group and The Osteoporosis Research Advisory Group. Meta-analyses of therapies for postmenopausal osteoporosis. VII. Meta-analysis of calcium supplementation for the prevention of postmenopausal osteoporosis’, Endocr Rev., vol. 23, no. 4, pp. 552-559.
Washington University School of Medicine 2007, ‘Dietary Calcium Is Better Than Supplements At Protecting Bone Health’, ScienceDaily, Retrieved October 25, 2010, from http://www.sciencedaily.com/releases/2007/06/070614112433.htm
Weaver et al. 2009, ‘Dairy vs Calcium Carbonate in Promoting Peak Bone Mass and Bone Maintenance During Subsequent Calcium Deficiency’, Journal of Bone and Mineral Research, 090323104508033 DOI: 10.1359/jbmr.090303